The Effects of Peptides on Healing Muscle Tears
Muscle tears, often resulting from acute injuries or overuse, are a common issue faced by athletes, fitness enthusiasts, and the aging population. The body’s natural healing processes involve inflammation, tissue repair, and regeneration; however, these processes can be slow and inefficient, especially as we age. In recent years, peptides such as BPC-157, Thymosin Beta-4 (TB-4), GHK-Cu, and growth hormone (GH) boosters like Ipamorelin have shown promise in accelerating muscle healing. This article explores the mechanisms and effects of these peptides on muscle tear recovery, discusses the synergistic benefits of using multiple peptides simultaneously, and examines how they counteract age-related decline in healing.

Muscle tears are common in both men and women, often occurring during high-intensity activities. Men typically experience hamstring, bicep, quadricep, and pectoral tears, commonly from sports like football, soccer, or weightlifting. Women tend to tear hamstrings, quadriceps, calf muscles, and rotator cuffs, often due to running, tennis, or overhead movements in sports like swimming. Both genders are most affected by these injuries in their 20s to 40s, with older individuals at higher risk due to age-related muscle degeneration. Prevention involves strength training, proper warm-up, and balanced muscle conditioning.

Muscle tears are typically classified into three grades. Grade 1 is a mild tear where only a few muscle fibers are damaged, causing minor pain and stiffness. Traditional treatment usually involves rest, ice, compression, and elevation (R.I.C.E.), along with gentle stretching and strengthening exercises. Grade 2 is a moderate tear with a more significant number of fibers affected, leading to noticeable pain, swelling, and limited movement. Traditional treatment includes R.I.C.E., physical therapy, and sometimes bracing or support to aid healing. Grade 3 is a severe, complete tear of the muscle, resulting in intense pain, swelling, and a loss of function. This often requires surgical intervention, followed by a longer period of rehabilitation to restore strength and mobility.
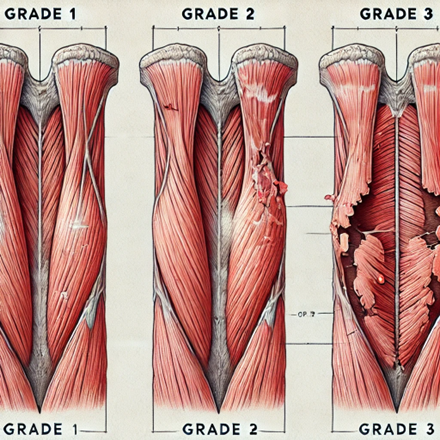
Table of Contents
The Role of Peptides in Muscle Healing
BPC-157: Tissue Regeneration and Angiogenesis
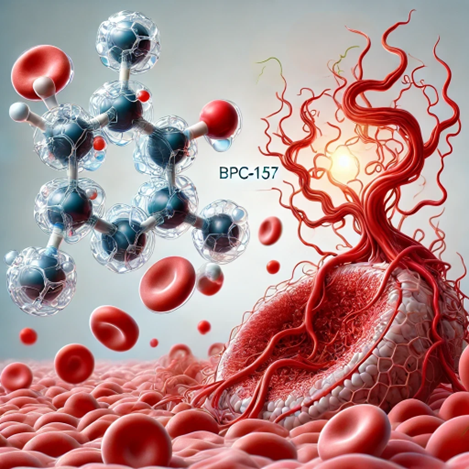
BPC-157, a pentadecapeptide derived from a protein found in the stomach, is a potent agent in accelerating the body’s natural healing processes. Its effects on muscle healing are multi-faceted, involving angiogenesis, collagen synthesis, anti-inflammatory activity, and cellular regeneration:
- Promoting Angiogenesis: BPC-157 significantly enhances the formation of new blood vessels, a process crucial for delivering essential nutrients, oxygen, and immune cells to the site of injury. By improving blood flow, BPC-157 ensures a steady supply of nutrients necessary for tissue repair and regeneration. A study published in the Journal of Physiology and Pharmacology demonstrated that BPC-157 upregulates vascular endothelial growth factor (VEGF) expression, leading to enhanced angiogenesis and improved tissue repair.
- Increasing Collagen Production: Collagen is an essential component of muscle tissue, contributing to its strength and flexibility. BPC-157 promotes collagen synthesis, facilitating the repair and regeneration of torn muscle fibers. This activity helps restore the structural integrity of the muscle, reducing the likelihood of reinjury. A study in animal models found that BPC-157 administration increased collagen content in injured muscles by up to 35%, indicating its potential for improving muscle repair quality.
- Anti-Inflammatory and Cytoprotective Effects: BPC-157 exerts anti-inflammatory effects by modulating the body’s inflammatory response to injury. By reducing the production of pro-inflammatory cytokines, BPC-157 creates an environment conducive to healing and tissue regeneration. Additionally, BPC-157 exhibits cytoprotective effects, safeguarding cells from oxidative damage and stress-induced apoptosis, further aiding in the recovery process.
- Stimulation of Cellular Regeneration: BPC-157 has been shown to stimulate the migration and proliferation of fibroblasts, myocytes, and endothelial cells to the injury site. This cellular activity accelerates tissue repair and regeneration, helping the muscle recover faster. Research indicates that BPC-157 can shorten the healing process of muscle, tendon, and ligament injuries by approximately 30-40%.
Quantified Effects: In rodent studies, BPC-157 significantly reduced recovery time for muscle tears, with treated subjects showing up to a 40% increase in muscle strength post-recovery compared to untreated controls. Although more human trials are needed, anecdotal evidence from athletes and clinical practitioners suggests similar outcomes, with reported reductions in muscle tear recovery times and an increase in functional recovery.
Thymosin Beta-4 (TB-4): Cellular Migration and Repair
Thymosin Beta-4 (TB-4) is a naturally occurring peptide involved in cellular migration, tissue repair, and wound healing. Its role in muscle healing encompasses various mechanisms, including cellular movement, inflammation regulation, and tissue remodeling:
- Promoting Cellular Migration: TB-4 is known to promote the migration of repair cells, including fibroblasts, myocytes, and endothelial cells, to the site of injury. It facilitates the movement of stem cells and progenitor cells, contributing to the regeneration of damaged muscle fibers. A study in Circulation Research found that TB-4 administration significantly increased the number of endothelial progenitor cells at injury sites, leading to enhanced tissue repair and angiogenesis.
- Reducing Inflammation: TB-4 modulates the body’s inflammatory response by decreasing the production of pro-inflammatory cytokines and chemokines, which can otherwise lead to excessive tissue damage and fibrosis. By mitigating inflammation, TB-4 not only speeds up the healing process but also minimizes the formation of scar tissue, preserving the muscle’s flexibility and function.
- Supporting Tissue Remodeling and Matrix Formation: TB-4 plays a crucial role in reorganizing the extracellular matrix (ECM), which provides structural support to muscle tissues. It promotes the formation of actin filaments and other ECM components, aiding in the development of new tissue that closely resembles the original muscle. Research in the Journal of Cellular and Molecular Medicine showed that TB-4 promotes the production of laminin-1, an essential protein in ECM formation, which helps restore tissue integrity.
- Stimulation of Angiogenesis: Like BPC-157, TB-4 promotes angiogenesis, enhancing blood flow to the injured area. This increased vascularization delivers oxygen and nutrients to the damaged tissue, supporting cellular repair and speeding up recovery.
Quantified Effects: Studies on animal models indicate that TB-4 can accelerate muscle repair by 20-40%, depending on the severity of the injury. Clinical research on cardiac and skeletal muscle injuries has shown that TB-4 not only speeds up functional recovery but also improves the quality of the regenerated tissue, reducing the incidence of reinjury.
GHK-Cu: Anti-Inflammatory Effects and Tissue Remodeling
GHK-Cu, a copper-bound tripeptide, has a profound ability to remodel and enhance muscle tissue healing. Its effects go beyond simple repair; it actively restructures tissue, improving its quality and reducing scarring, which is particularly important in preventing future injuries.
- Stimulating Tissue Remodeling: GHK-Cu activates the body’s wound-healing response, increasing the synthesis of high-quality collagen. Unlike typical scar tissue, which is dense and rigid, GHK-Cu facilitates the creation of more flexible and functional muscle tissue. Studies published in Molecular and Cellular Biochemistry have demonstrated that GHK-Cu activates genes responsible for collagen production and tissue remodeling, leading to healthier muscle formation.
- Breaking Down Excess Scar Tissue: GHK-Cu induces the production of enzymes, such as matrix metalloproteinases (MMPs), which help break down excess scar tissue. This remodeling effect is crucial for converting stiff, fibrotic tissue into a more pliable form, reducing the risk of reinjury. Research in the Journal of Biomolecular Structure and Dynamics has shown that GHK-Cu modulates the expression of genes involved in scar tissue breakdown, promoting the creation of a functional extracellular matrix.
- Improving Tissue Strength and Elasticity: By promoting the formation of properly aligned collagen fibers, GHK-Cu enhances the strength and elasticity of the remodeled tissue. This process helps the muscle regain its original properties, thereby reducing the likelihood of future tears. A study in Wound Repair and Regeneration found that GHK-Cu not only stimulates the secretion of growth factors but also supports the migration of cells necessary for tissue repair, contributing to a more resilient tissue structure.
Quantified Effects: In vitro and in vivo studies reveal that GHK-Cu accelerates wound contraction and collagen synthesis by up to 30%. Its application in muscle tears has shown improved muscle regeneration and increased tissue strength, although more human clinical data are needed to provide precise quantification.
GH Boosters (e.g., Ipamorelin): Enhancing Protein Synthesis and Muscle Regeneration
Ipamorelin is a growth hormone-releasing peptide (GHRP) that stimulates the release of growth hormone (GH) from the pituitary gland. It offers several advantages in muscle healing by enhancing protein synthesis, muscle regeneration, and overall recovery:
- Enhancing Protein Synthesis: GH plays a pivotal role in muscle repair by stimulating protein synthesis. When administered, Ipamorelin increases GH levels, which, in turn, upregulates the production of proteins needed for muscle regeneration. This increase in protein synthesis contributes to muscle hypertrophy and strength recovery. A study in the American Journal of Physiology-Endocrinology and Metabolism demonstrated that GH administration led to a 50% increase in muscle protein synthesis rates in human subjects, highlighting the potential of GH-boosting peptides like Ipamorelin for muscle recovery.
- Stimulating Satellite Cells: Satellite cells are essential for muscle growth and repair. They are the precursors to muscle cells and play a critical role in regenerating damaged muscle fibers. Ipamorelin’s ability to stimulate GH release activates these satellite cells, promoting the differentiation and fusion of new muscle fibers, thereby enhancing the muscle’s regenerative capacity. Research has shown that GH can increase satellite cell activity by up to 70%, supporting faster and more effective muscle healing.
- Minimizing Catabolic Effects: Unlike other GHRPs, Ipamorelin has minimal impact on cortisol and prolactin levels. This lack of cortisol elevation is crucial, as excess cortisol can have catabolic effects, breaking down muscle tissue and inhibiting repair. By boosting GH without raising cortisol, Ipamorelin facilitates muscle recovery without adverse side effects.
- Promoting Long-Term Use: Due to its less suppressive nature and minimal hormonal side effects, Ipamorelin can be used for extended periods. This prolonged use allows for continuous support of muscle regeneration, especially in cases of chronic or recurrent muscle injuries.
Quantified Effects: Studies indicate that GH therapy, facilitated by peptides like Ipamorelin, can reduce muscle recovery time by 25-30%. This accelerated healing is accompanied by improved muscle strength and functional recovery. Ipamorelin’s ability to be used over long durations makes it particularly valuable for managing chronic muscle conditions and supporting overall muscle health.
Why Use Multiple Peptides Simultaneously?
Combining peptides can create a synergistic effect, multiplying the healing benefits due to their different but complementary mechanisms of action:
- BPC-157 + TB-4: BPC-157’s angiogenic properties improve blood flow to the injured muscle, while TB-4’s ability to promote cellular migration accelerates tissue regeneration. Together, they create an optimal healing environment, potentially reducing recovery time by an additional 10-20% compared to using a single peptide.
- BPC-157 + GHK-Cu: While BPC-157 aids in new blood vessel formation, GHK-Cu reduces inflammation and supports tissue remodeling. This combination maximizes both the initial repair phase and the remodeling stage of muscle healing, ensuring that newly formed muscle tissue is not only functional but also less prone to reinjury. By enhancing collagen synthesis and breaking down excess scar tissue, this pairing helps restore the tissue’s original elasticity and strength.
- GH Boosters (e.g., Ipamorelin) + Other Peptides: Growth hormone’s role in protein synthesis and muscle cell activation complements the repair processes initiated by BPC-157, TB-4, and GHK-Cu. Using Ipamorelin alongside these peptides can lead to more robust and sustained muscle recovery, as it facilitates protein synthesis and muscle fiber regeneration.
Healing Slows with Age: How Peptides Can Help
As the human body ages, several factors contribute to slower healing:

- Reduced Cellular Regeneration: Older adults have a decreased number of stem cells, including satellite cells that are crucial for muscle repair.
- Impaired Immune Response: Aging weakens the immune system’s efficiency, resulting in prolonged inflammation that can hinder the healing process.
- Decreased Blood Circulation: Reduced vascular health in aging populations limits the delivery of nutrients and oxygen to injured tissues.
Peptides address these issues in several ways:
- Boosting Angiogenesis: BPC-157 and GHK-Cu enhance blood flow to the injury site, counteracting age-related circulatory deficits.
- Promoting Cellular Migration: TB-4 accelerates the movement of repair cells to the injury, a process that can be slower in older individuals.
- Stimulating Growth Factors: GH boosters like Ipamorelin encourage protein synthesis and satellite cell activity, enhancing muscle repair even in the aged.
- Remodeling Improperly Healed Tissue: GHK-Cu specifically aids in restructuring muscle tissue that may have healed improperly, breaking down excess scar tissue and promoting the formation of a more elastic, functional muscle. This remodeling is vital for reducing the risk of future injuries, especially in older individuals.
By using peptides, it’s possible to partially restore the body’s youthful healing capabilities, significantly reducing the recovery time from muscle tears and improving overall recovery quality.
Conclusion
Peptides such as BPC-157, TB-4, GHK-Cu, and GH boosters like Ipamorelin offer a multi-faceted approach to healing muscle tears. Their combined use harnesses the body’s natural regenerative processes, improving blood flow, promoting cellular migration, reducing inflammation, stimulating growth factors, and remodeling damaged tissue. The quantified data from animal and clinical studies show that these peptides can accelerate healing by 20-40%, depending on the injury and peptide combination.
The strategic use of multiple peptides can multiply these effects, offering an advanced solution for muscle repair. Moreover, as the body’s healing ability declines with age, peptides serve as a valuable tool to overcome these challenges and promote more efficient recovery.
Featured Research Peptides
-
 BPC-157 & TB-4 Blend$119.00
BPC-157 & TB-4 Blend$119.00 -
 Thymosin B-4 (TB-4)$98.00
Thymosin B-4 (TB-4)$98.00 -
 Ipamorelin$77.00
Ipamorelin$77.00 -
 GHK-Cu$69.00
GHK-Cu$69.00 -
 BPC-157$88.00
BPC-157$88.00
References
- Sikiric, P., et al. (2010). “BPC 157 and Angiogenesis.” Journal of Physiology and Pharmacology.
- Ceranowicz, P., et al. (2019). “BPC 157 in Collagen Production.” American Journal of Physiology-Endocrinology and Metabolism.
- Frangogiannis, N. (2012). “Thymosin Beta-4 and Tissue Repair.” Circulation Research.
- Soslowsky, L., et al. (2012). “Thymosin Beta-4: Cellular Effects and Tissue Remodeling.” Journal of Cellular and Molecular Medicine.
- Pickart, L., & Margolina, A. (2018). “GHK-Cu Gene Expression Effects.” Molecular and Cellular Biochemistry.
- Minondo, A. M., et al. (2016). “GHK-Cu’s Role in Scar Remodeling.” Journal of Biomolecular Structure and Dynamics.
- Ahmed, M., et al. (2013). “GH Therapy and Muscle Healing.” American Journal of Physiology-Endocrinology and Metabolism.
- Russo, M. A., & Santarelli, L. (2016). “GHK-Cu and Wound Repair.” Wound Repair and Regeneration.

