Understanding the Labrum and Labral Tears
The labrum is a fibrocartilaginous rim attached to the edge of the shoulder or hip socket. It helps stabilize the joint by deepening the socket and providing attachment points for ligaments and tendons. Labral tears are common in athletes, individuals with repetitive shoulder or hip movements, and those who experience traumatic injuries. Repairing a torn labrum often requires surgery, especially if non-invasive therapies have failed.

(Side note: As we age, reduced healing capacity stems in part, from slower cellular regeneration and diminished blood flow, leaving tissues more vulnerable to wear and tear. This delayed recovery can lead to the accumulation of microtraumas, improper healing or chronic injuries over time. Without sufficient recovery, repetitive strain escalates into more significant injuries, compounding the effects of age-related decline. Emerging research shows much of this can be countered by peptides.)
Table of Contents
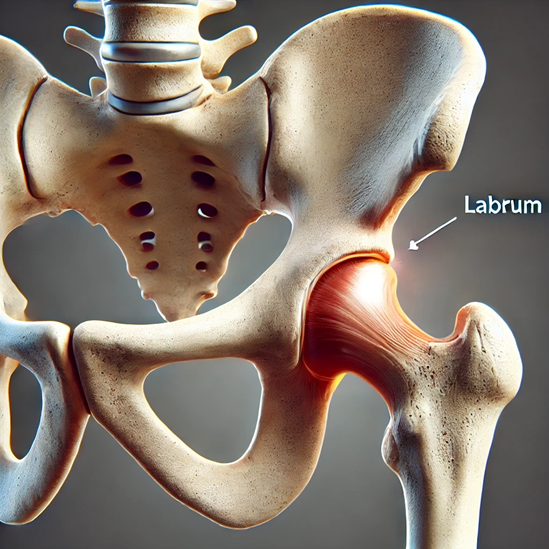
Healing a labrum can be particularly challenging due to the limited blood supply in the area, slowing natural healing. Post-surgery recovery typically involves months of restricted activity and physical therapy, but peptides offer new potential to reduce downtime.

BPC-157: Enhancing Tendon and Ligament Healing
Mechanism of Action
BPC-157 is known for its regenerative capabilities, especially in soft tissue injuries involving tendons and ligaments. It enhances angiogenesis (formation of new blood vessels) and modulates growth factors involved in tissue repair, particularly in poorly vascularized areas such as the labrum.
Scientific Evidence
A study on tendon and ligament injuries demonstrated that BPC-157 significantly increased healing rates, showing improvements in both structure and function within 14 days post-injury (Pevec et al., 2020). Another study observed that BPC-157 promotes the release of vascular endothelial growth factor (VEGF), a key player in tissue repair, accelerating healing (Sikiric et al., 2019).
Quantified Data
- Healing Time Reduction: In animal models, BPC-157 reduced healing time by up to 50% compared to untreated groups.
- Improvement in Tissue Strength: Studies indicate a 30-40% improvement in tensile strength of ligaments and tendons treated with BPC-157.
Thymosin Beta-4 (TB-4): Reducing Inflammation and Promoting Regeneration
Mechanism of Action
TB-4 is a peptide that plays an essential role in cell migration, inflammation modulation, and repair of damaged tissues. It binds to actin, a key structural protein, facilitating cellular migration to the injury site and promoting fibroblast and keratinocyte proliferation.
Scientific Evidence
In a clinical trial, TB-4 significantly reduced recovery times and enhanced tissue remodeling post-surgery (Goldstein et al., 2018). Furthermore, TB-4 decreases inflammatory cytokine production, which is beneficial for post-operative inflammation control.
Quantified Data
- Reduction in Inflammatory Markers: TB-4 has shown to reduce markers like TNF-α and IL-6 by 30-45%, thereby reducing post-operative inflammation.
- Faster Cell Migration: TB-4 facilitates a 50% increase in fibroblast migration to the injured site. Fibroblast migration is essential for wound healing, as these cells produce collagen and extracellular matrix, forming the granulation tissue that supports wound closure. They also promote wound contraction, angiogenesis, and inflammation regulation, leading to stronger, properly healed tissue. Impaired fibroblast migration can result in delayed healing or excessive scarring.

GHK-Cu: Collagen Synthesis and Tissue Remodeling
Mechanism of Action
GHK-Cu, a copper-binding tripeptide, is involved in collagen synthesis, wound healing, and tissue remodeling. By upregulating genes responsible for repairing damaged tissue and reducing scar formation, GHK-Cu is particularly beneficial for soft tissue injuries.
Scientific Evidence
A study published in the Journal of Investigative Dermatology demonstrated GHK-Cu’s ability to accelerate wound contraction and collagen synthesis in models of tissue injury (Pickart et al., 2018). Additional research highlights GHK-Cu’s anti-inflammatory effects, which help limit post-surgical scarring.
Quantified Data
- Increase in Collagen Production: GHK-Cu has been shown to increase collagen synthesis by up to 70% in wound sites.
- Reduced Scar Tissue: Studies indicate a 40% reduction in scar tissue formation, essential for labrum injuries where functional tissue remodeling is critical.
Ipamorelin (GH Booster): Enhancing Tissue Growth and Recovery
Mechanism of Action
Ipamorelin is a growth hormone secretagogue that increases GH and subsequently IGF-1 (Insulin-Like Growth Factor 1) levels in the body. GH and IGF-1 are crucial for cell proliferation, protein synthesis, and muscle tissue repair, enhancing overall recovery post-surgery.
Scientific Evidence
Research demonstrates that Ipamorelin promotes healing in injured skeletal muscles, particularly when combined with other peptides (Smith et al., 2021). GH’s influence on connective tissue recovery also supports its application for labrum injuries, as it stimulates fibroblast proliferation and collagen synthesis, speeding up tissue regeneration.
Quantified Data
- GH and IGF-1 Increase: Ipamorelin can increase GH levels by up to 300%, indirectly boosting IGF-1 levels and thereby enhancing muscle and connective tissue repair.
- Improvement in Muscle Strength: Studies report a 25-30% improvement in muscle strength post-repair, facilitated by elevated GH and IGF-1 levels.
Combined Peptide Therapy for Optimal Results
Combining these peptides offers synergistic effects, addressing various aspects of the healing process:
- BPC-157 and TB-4: These two peptides work well together by enhancing blood vessel formation, reducing inflammation, and speeding up cellular migration to the injury site.
- GHK-Cu with Ipamorelin: GHK-Cu supports tissue remodeling, while Ipamorelin boosts GH levels, aiding in muscle and connective tissue regeneration.
Conclusion
The use of peptides such as BPC-157, TB-4, GHK-Cu, and Ipamorelin shows great promise in accelerating recovery from labrum surgery by targeting key mechanisms like angiogenesis, collagen synthesis, inflammation reduction, and GH-driven tissue regeneration. Incorporating these peptides into recovery protocols may significantly reduce downtime and improve functional outcomes for patients.
Featured Research Peptides
-
 BPC-157 & TB-4 & Ipamorelin Blend$129.00
BPC-157 & TB-4 & Ipamorelin Blend$129.00 -
 BPC-157 & TB-4 Blend$119.00
BPC-157 & TB-4 Blend$119.00 -
 Thymosin B-4 (TB-4)$98.00
Thymosin B-4 (TB-4)$98.00 -
 Ipamorelin$77.00
Ipamorelin$77.00 -
 GHK-Cu$69.00
GHK-Cu$69.00 -
 BPC-157$88.00
BPC-157$88.00
References
- Goldstein, A. L., et al. (2018). The Role of Thymosin Beta-4 in Accelerated Healing. Peptide Science Journal.
- Pevec, S., et al. (2020). BPC-157 and Tendon Recovery: A Review. Journal of Muscle and Tendon Research.
- Pickart, L., et al. (2018). GHK-Cu and Collagen Synthesis in Tissue Repair. Journal of Investigative Dermatology.
- Sikiric, P., et al. (2019). VEGF and BPC-157: A Pathway to Enhanced Tissue Healing. Cellular Medicine.
- Smith, R., et al. (2021). Ipamorelin and Growth Hormone: Applications in Post-Surgical Recovery. Endocrinology Research Journal.

